Essential Osteoporosis Management for the Primary Care Provider
DOI:
https://doi.org/10.58931/cpct.2024.2228Abstract
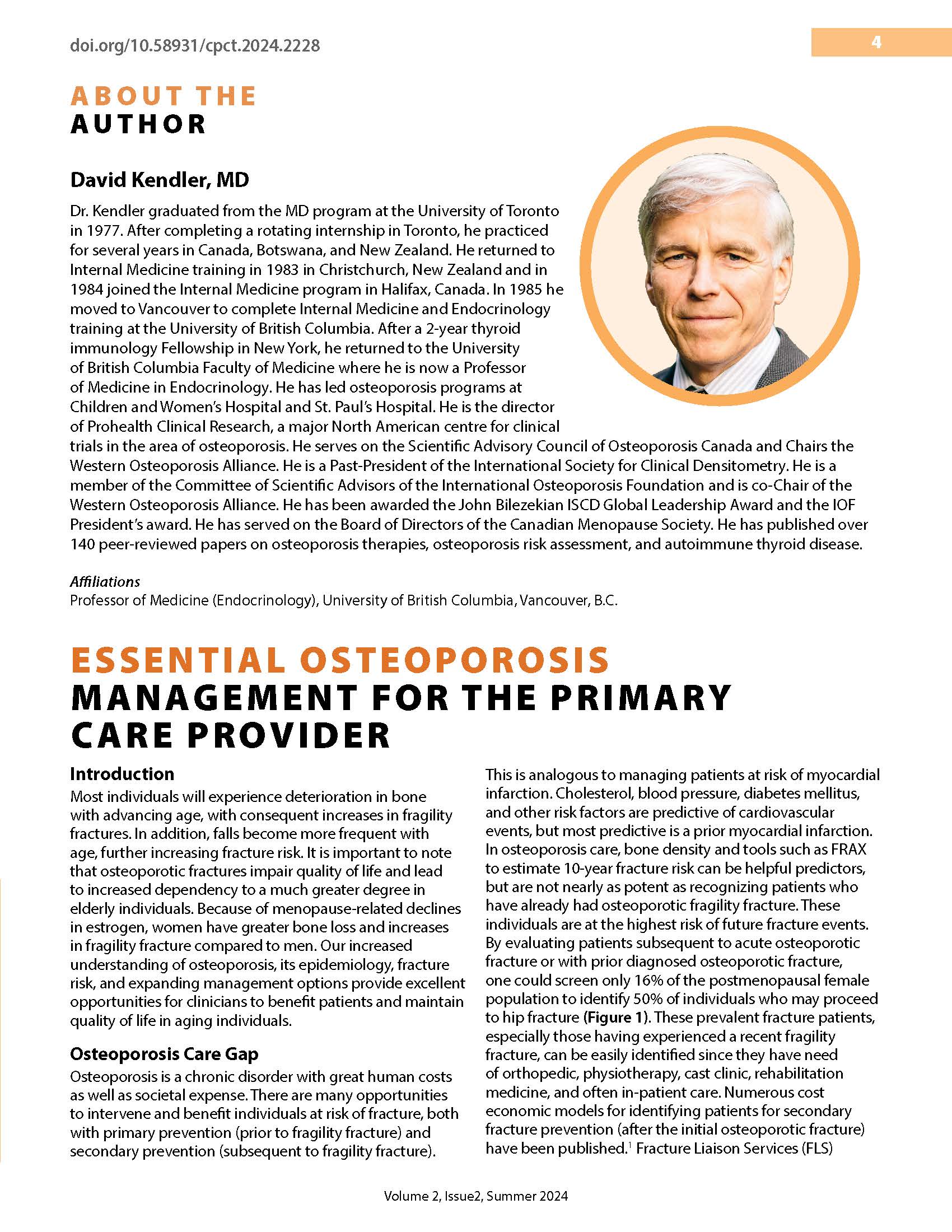
Most individuals will experience deterioration in bone with advancing age, with consequent increases in fragility fractures. In addition, falls become more frequent with age, further increasing fracture risk. It is important to note that osteoporotic fractures impair quality of life and lead to increased dependency to a much greater degree in elderly individuals. Because of menopause-related declines in estrogen, women have greater bone loss and increases in fragility fracture compared to men. Our increased understanding of osteoporosis, its epidemiology, fracture risk, and expanding management options provide excellent opportunities for clinicians to benefit patients and maintain quality of life in aging individuals.
References
Danazumi MS, Lightbody N, Dermody G. Online effectiveness of fracture liaison service in reducing the risk of secondary fragility fractures in adults aged 50 and older: a systematic review and meta-analysis. Osteoporos Int. 2024 Mar 27. DOI: https://doi.org/10.1007/s00198-024-07052-1
Ross AC, Manson JE, Abrams SA, et al. The 2011 Report on dietary reference intakes for calcium and vitamin d from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011 Jan; 96(1): 53-8. DOI: https://doi.org/10.1016/j.jada.2011.01.004
https://osteoporosis.ca/exercise-recommendations/.
Adachi JD, Brown JP, Schemitsch E, et al. Fragility fracture identifies patients at imminent risk for subsequent fracture: real-world perspective database study in Ontario, Canada. BMC Muscoloskelet Disord. 2021 Feb 26;22(1):224. DOI: https://doi.org/10.1186/s12891-021-04051-9
Real-world retrospective database study in Ontario, Canada. BMC Musculoskelet Disord. 2021;22:224.
Balasubramanian A, Zhang J, Chen L, et al. Risk of subsequent fracture after prior fracture among older women. Osteoporos Int. 2019;30:79-92. DOI: https://doi.org/10.1007/s00198-018-4732-1
Johansson H, Siggeirsdottir K, Harvey NC, et al. Imminent risk of fracture after fracture. Osteoporos Int. 2017;28:775-80. DOI: https://doi.org/10.1007/s00198-016-3868-0
Camacho PM. American Association of Clinical Endocrinologists/American College of Endocrinology Clinical Practice Guidelines for the Diagnosis and Treatment of Postmenopausal Osteoporosis—2020 Update. Endocrine Practice. 2020 May;26(Suppl 1):1-46. DOI: https://doi.org/10.4158/GL-2020-0524SUPPL
Kendler DL, Cosman F, Stad RK, et al. Denosumab in the treatment of osteoporosis: 10 years later: a narrative review. Adv Ther. 2022;39:58-74. DOI: https://doi.org/10.1007/s12325-021-01936-y
Cosman F, Kendler DL, Langdahl BL, et al. Romosozumab and antiresorptive treatment: the importance of treatment sequence. Osteoporos Int. 2022;33:1243-56. DOI: https://doi.org/10.1007/s00198-021-06174-0
Adler RA et al. Managing osteoporosis in patients on long-term bisphosphonate treatment: report of a task force of the American Society for Bone and Mineral Research. Journal of Bone and Mineral Research. 2016;31(1):16–35. DOI: https://doi.org/10.1002/jbmr.2708
Black DM, Geiger EJ, Eastell R, et al. Atypical femur fracture risk versus fragility fracture prevention with bisphosphonates. N Engl J Med. 2020;383:743-53). DOI: https://doi.org/10.1056/NEJMoa1916525
Brankin E, Mitchell C, Monroe R & on behalf of Lanarkshire Osteoporosis Service. Curr Med Res Opin. 2005;21:4:475-82. DOI: https://doi.org/10.1185/030079905X38150
https://www.asbmr.org/about/news-release-detail/press-release-asbmr-coalition-clinical-recommendat.
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Canadian Primary Care Today

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.