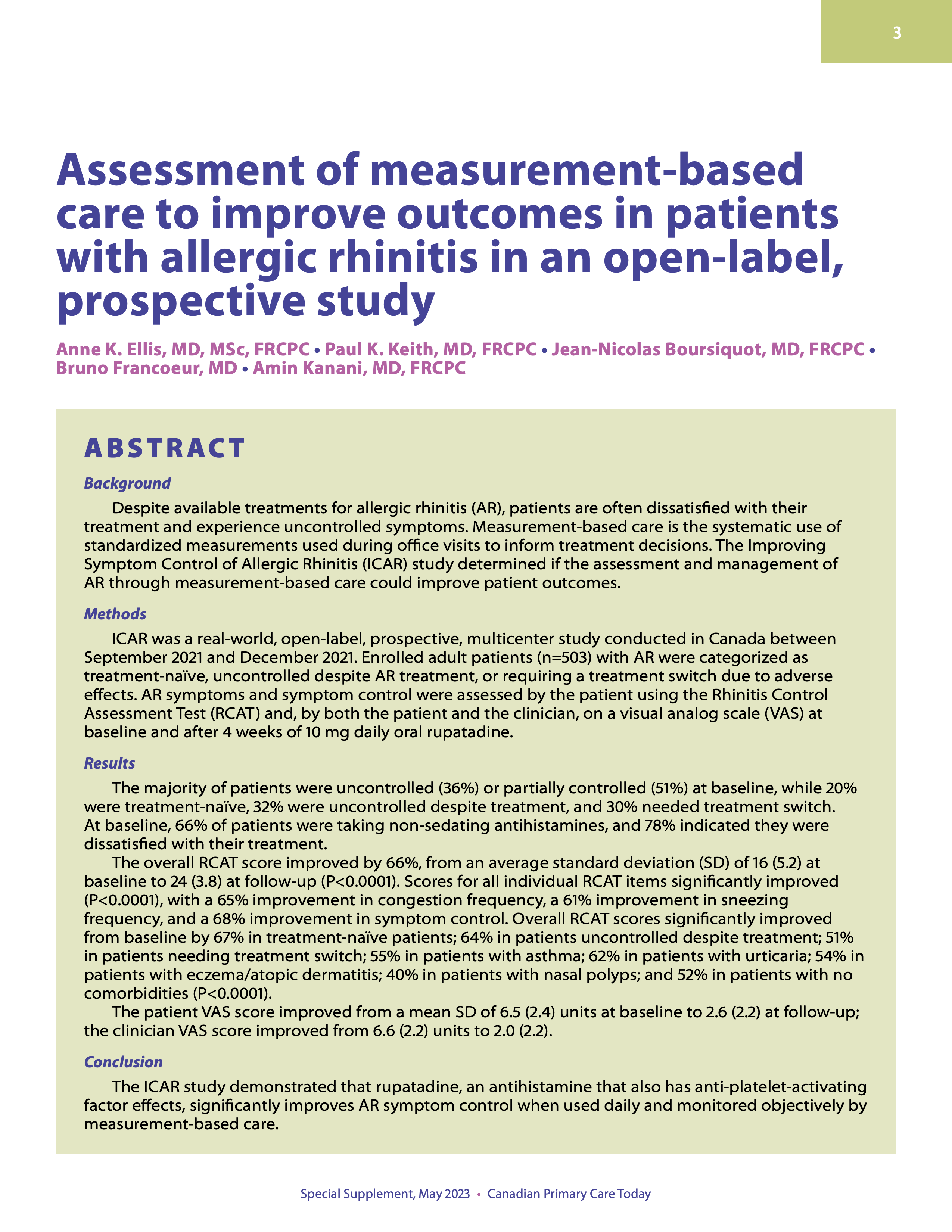
Assessment of measurement-based care to improve outcomes in patients with allergic rhinitis in an open-label, prospective study
DOI:
https://doi.org/10.58931/cpct.2023.1S0511Abstract
Background
Despite available treatments for allergic rhinitis (AR), patients are often dissatisfied with their treatment and experience uncontrolled symptoms. Measurement-based care is the systematic use of standardized measurements used during office visits to inform treatment decisions. The Improving Symptom Control of Allergic Rhinitis (ICAR) study determined if the assessment and management of AR through measurement-based care could improve patient outcomes.
MethodsICAR was a real-world, open-label, prospective, multicenter study conducted in Canada between September 2021 and December 2021. Enrolled adult patients (n=503) with AR were categorized as treatment-naïve, uncontrolled despite AR treatment, or requiring a treatment switch due to adverse effects. AR symptoms and symptom control were assessed by the patient using the Rhinitis Control Assessment Test (RCAT) and, by both the patient and the clinician, on a visual analog scale (VAS) at baseline and after 4 weeks of 10 mg daily oral rupatadine.
ResultsThe majority of patients were uncontrolled (36%) or partially controlled (51%) at baseline, while 20% were treatment-naïve, 32% were uncontrolled despite treatment, and 30% needed treatment switch.
At baseline, 66% of patients were taking non-sedating antihistamines, and 78% indicated they were dissatisfied with their treatment.
The overall RCAT score improved by 66%, from an average standard deviation (SD) of 16 (5.2) at baseline to 24 (3.8) at follow-up (P<0.0001). Scores for all individual RCAT items significantly improved (P<0.0001), with a 65% improvement in congestion frequency, a 61% improvement in sneezing frequency, and a 68% improvement in symptom control. Overall RCAT scores significantly improved from baseline by 67% in treatment-naïve patients; 64% in patients uncontrolled despite treatment; 51% in patients needing treatment switch; 55% in patients with asthma; 62% in patients with urticaria; 54% in patients with eczema/atopic dermatitis; 40% in patients with nasal polyps; and 52% in patients with no comorbidities (P<0.0001).
The patient VAS score improved from a mean SD of 6.5 (2.4) units at baseline to 2.6 (2.2) at follow-up; the clinician VAS score improved from 6.6 (2.2) units to 2.0 (2.2).
ConclusionThe ICAR study demonstrated that rupatadine, an antihistamine that also has anti-platelet-activating factor effects, significantly improves AR symptom control when used daily and monitored objectively by measurement-based care.
References
Meltzer EO, Blaiss MS, Naclerio RM, Stoloff SW, Derebery MJ, Nelson HS, et al. Burden of allergic rhinitis: Allergies in America, Latin America, and Asia-Pacific adult surveys. Allergy Asthma Proc. 2012;33 Suppl 1:S113-41. DOI: https://doi.org/10.2500/aap.2012.33.3603
Meltzer EO, Farrar JR, Sennett C. Findings from an online survey assessing the burden and management of seasonal allergic rhinoconjunctivitis in US patients. The Journal of Allergy and Clinical Immunology: In Practice. 2017 May 1;5(3):779-89. DOI: https://doi.org/10.1016/j.jaip.2016.10.010
Keith PK, Desrosiers M, Laister T, Schellenberg RR, Waserman S. The burden of allergic rhinitis (AR) in Canada: perspectives of physicians and patients. Allergy, Asthma & Clinical Immunology. 2012 Dec;8(1):1-1. DOI: https://doi.org/10.1186/1710-1492-8-7
Cingi C, Gevaert P, Mösges R, Rondon C, Hox V, Rudenko M, Muluk NB, Scadding G, Manole F, Hupin C, Fokkens WJ. Multi-morbidities of allergic rhinitis in adults: European acad- emy of allergy and clinical immunology task force report. Clinic- al and Translational Allergy. 2017 Dec;7(1):1-2. DOI: https://doi.org/10.1186/s13601-017-0153-z
Church MK, Máspero JF, Maurer M, Ryan D, Canonica GW, Baena-Cagnani CE. The scope of pharmacological and clinical effects of modern antihistamines, with a special focus on rupatadine: proceedings from a satellite symposium held at the 21st World Allergy Congress, Buenos Aires, December 8, 2009. The World Allergy Organization Journal. 2010 Apr;3(Suppl 1):S1. DOI: https://doi.org/10.1186/1939-4551-3-S1-S1
Rosenwasser L. New insights into the pathophysiology of allergic rhinitis. Allergy and Asthma Proceedings. 2007;28:10-5. DOI: https://doi.org/10.2500/aap.2007.28.2977
Brożek JL, Bousquet J, Agache I, Agarwal A, Bachert C, Bos- nic-Anticevich S, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines-2016 revision. J Allergy Clin Immunol. 2017;140:950-8. DOI: https://doi.org/10.1016/j.jaci.2017.03.050
Hossenbaccus L, Linton S, Garvey S, Ellis AK. Towards definitive management of allergic rhinitis: best use of new and estab- lished therapies. Allergy, Asthma & Clinical Immunology. 2020 Dec;16(1):1-7. DOI: https://doi.org/10.1186/s13223-020-00436-y
Small P, Keith PK, Kim H. Allergic rhinitis. Allergy, Asthma & Clin- ical Immunology. 2018 Sep;14(2):1-1. DOI: https://doi.org/10.1186/s13223-018-0280-7
Dykewicz MS, Wallace DV, Amrol DJ, Baroody FM, Bernstein JA, Craig TJ, Dinakar C, Ellis AK, Finegold I, Golden DB, Greenhawt MJ. Rhinitis 2020: a practice parameter update. Journal of Al- lergy and Clinical Immunology. 2020 Oct 1;146(4):721-67. DOI: https://doi.org/10.1016/j.jaci.2020.07.007
Jeffrey J, Klomhaus A, Enenbach M, Lester P, Krishna R. Self-re- port rating scales to guide measurement-based care in child and adolescent psychiatry. Child and Adolescent Psychiatric Clinics. 2020 Oct 1;29(4):601-29. DOI: https://doi.org/10.1016/j.chc.2020.06.002
Aboraya A, Nasrallah HA, Elswick DE, Ahmed E, Estephan N, Aboraya D, et al. Measurement-based Care in Psychiatry-Past, Present, and Future. Innov Clin Neurosci. 2018;15:13-26.
Higdon C, Blader J, Kalari VK, Fornari VM. Measurement-Based Care in the Treatment of Attention-Deficit/Hyperactivity Disorder and Disruptive Behavior Disorders. Child and Adolescent Psychiatric Clinics. 2020 Oct 1;29(4):663-74. DOI: https://doi.org/10.1016/j.chc.2020.06.005
Waldrop J, McGuinness TM. Measurement-based care in psychiatry. Journal of Psychosocial Nursing and Mental Health Services. 2017 Nov 1;55(11):30-5. DOI: https://doi.org/10.3928/02793695-20170818-01
Meltzer EO, Schatz M, Nathan R, Garris C, Stanford RH, Kosinski M. Reliability, validity, and responsiveness of the Rhinitis Control Assessment Test in patients with rhinitis. Journal of Allergy and Clinical Immunology. 2013 Feb 1;131(2):379-86. DOI: https://doi.org/10.1016/j.jaci.2012.10.022
Simons FE, Simons KJ. Histamine and H1-antihistamines: celebrating a century of progress. Journal of Allergy and Clinical Immunology. 2011 Dec 1;128(6):1139-50. DOI: https://doi.org/10.1016/j.jaci.2011.09.005
Muñoz-Cano RM, Casas-Saucedo R, Valero Santiago A, Bobolea I, Ribó P, Mullol J. Platelet-activating factor (PAF) in allergic rhinitis: clinical and therapeutic implications. Journal of Clinical Medicine. 2019 Aug 29;8(9):1338. DOI: https://doi.org/10.3390/jcm8091338
Wong MM, Keith PK. Presence of positive skin prick tests to inhalant allergens and markers of T2 inflammation in subjects with chronic spontaneous urticaria (CSU): a systematic literature review. Allergy, Asthma & Clinical Immunology. 2020 Aug 4;16(1):72. DOI: https://doi.org/10.1186/s13223-020-00461-x
Keith PK, Luciuk G. Effectiveness of desloratadine 5 mg once daily in patients with symptoms of seasonal allergic rhinitis: results of a Canadian multicenter, open-label trial. Clinical Therapeutics. 2007 Mar 1;29(3):419-26. DOI: https://doi.org/10.1016/S0149-2918(07)80080-4
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Canadian Primary Care Today

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.